YOU MIGHT BE SUPRISED HOW COMMON LYMPHOMA IS
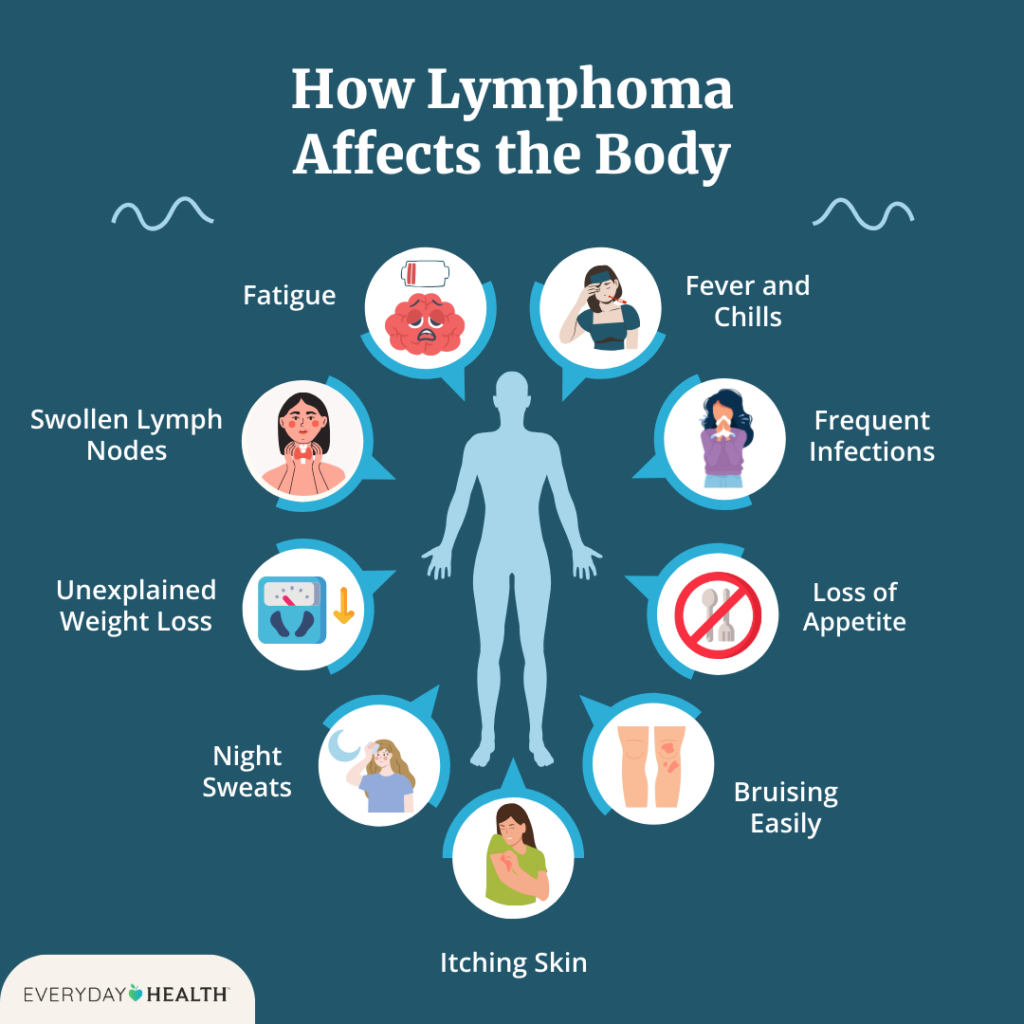
Lymphoma, a type of blood cancer that originates in the lymphatic system, is more prevalent than many might assume. The lymphatic system is a crucial part of the body’s immune system, comprising lymph nodes, the spleen, thymus gland, and bone marrow. Lymphoma occurs when lymphocytes, a type of white blood cell, grow uncontrollably, leading to the formation of tumors in lymph nodes or other parts of the lymphatic system. This essay will explore the prevalence of lymphoma, the reasons behind its commonality, the types of lymphoma, risk factors, diagnosis. Also, we will explore treatment options, and current research.
UNDERSTANDING LYMPHOMA.
Lymphoma is classified into two main categories: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). Hodgkin lymphoma is characterized by the presence of Reed-Sternberg cells, which are large, abnormal lymphocytes. Non-Hodgkin lymphoma, on the other hand, encompasses a diverse group of blood cancers that can arise from B-cells, T-cells, or natural killer (NK) cells. NHL is far more common than HL, accounting for about 90% of all lymphoma cases .
PREVALENCE OF LYMPHOMA.
Lymphoma is the seventh most common cancer in the United States, with an estimated 90,000 new cases diagnosed annually . It is also one of the most prevalent cancers worldwide, affecting approximately 500,000 people each year . The incidence of lymphoma has been steadily increasing over the past few decades, particularly in developed countries. This rise is partly due to improved diagnostic techniques, increased awareness, and a growing aging population, as the risk of lymphoma increases with age.
THE COMMONALITY OF LYMPHOMA: WHY IS IT SO PREVALENT?
There are several factors contributing to the commonality of lymphoma:
- Aging Population:
- As people age, their immune systems naturally weaken, making them more susceptible to cancers like lymphoma. Lymphoma is most commonly diagnosed in individuals aged 60 and older. The increasing average age of the global population is, therefore, a significant factor in the rising incidence of lymphoma.
- Immunodeficiency:
- Individuals with weakened immune systems are at a higher risk of developing lymphoma. This includes people with HIV/AIDS, those on immunosuppressive medications following organ transplants, and those with autoimmune diseases. As the prevalence of these conditions rises, so does the incidence of lymphoma.
- Environmental Factors:
- Exposure to certain chemicals and toxins, such as pesticides, herbicides, and industrial solvents, has been linked to an increased risk of lymphoma. Occupational exposure, especially in agricultural and manufacturing settings, contributes to the disease’s prevalence.
- Viral Infections:
- Certain viral infections are known to increase the risk of lymphoma. For example, the Epstein-Barr virus (EBV) is associated with Hodgkin lymphoma and certain types of non-Hodgkin lymphoma. Human T-cell leukemia/lymphoma virus (HTLV-1) is linked to adult T-cell leukemia/lymphoma, and the human immunodeficiency virus (HIV) increases the risk of NHL.
- Family History and Genetics:
- A family history of lymphoma or other cancers can increase an individual’s risk of developing the disease. Genetic predispositions, such as mutations in the BRCA1 and BRCA2 genes, have also been associated with a higher risk of lymphoma.
TYPES OF LYMPHOMA.
The two main types of lymphoma, Hodgkin lymphoma and non-Hodgkin lymphoma, have distinct characteristics and subtypes:
- Hodgkin Lymphoma (HL):
- Hodgkin lymphoma is relatively rare, accounting for about 10% of all lymphoma cases. It is most commonly diagnosed in young adults between the ages of 15 and 35, as well as in older adults over 55. There are two main subtypes of HL: classical Hodgkin lymphoma (cHL), which makes up about 95% of HL cases, and nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL), which is less common .
- Non-Hodgkin Lymphoma (NHL):
- Non-Hodgkin lymphoma is much more common than HL and includes a wide variety of subtypes. NHL can be categorized into B-cell lymphomas, which are the most common, and T-cell lymphomas. Some of the most prevalent subtypes of NHL include:
- Diffuse Large B-cell Lymphoma (DLBCL): The most common subtype of NHL, accounting for about 30% of all cases.
- Follicular Lymphoma: A slow-growing lymphoma that makes up about 20% of NHL cases.
- Mantle Cell Lymphoma: A rare and aggressive form of NHL, accounting for about 6% of cases.
- Peripheral T-cell Lymphoma (PTCL): A group of rare and aggressive T-cell lymphomas.
- Non-Hodgkin lymphoma is much more common than HL and includes a wide variety of subtypes. NHL can be categorized into B-cell lymphomas, which are the most common, and T-cell lymphomas. Some of the most prevalent subtypes of NHL include:
RISK FACTORS FOR LYMPHOMA
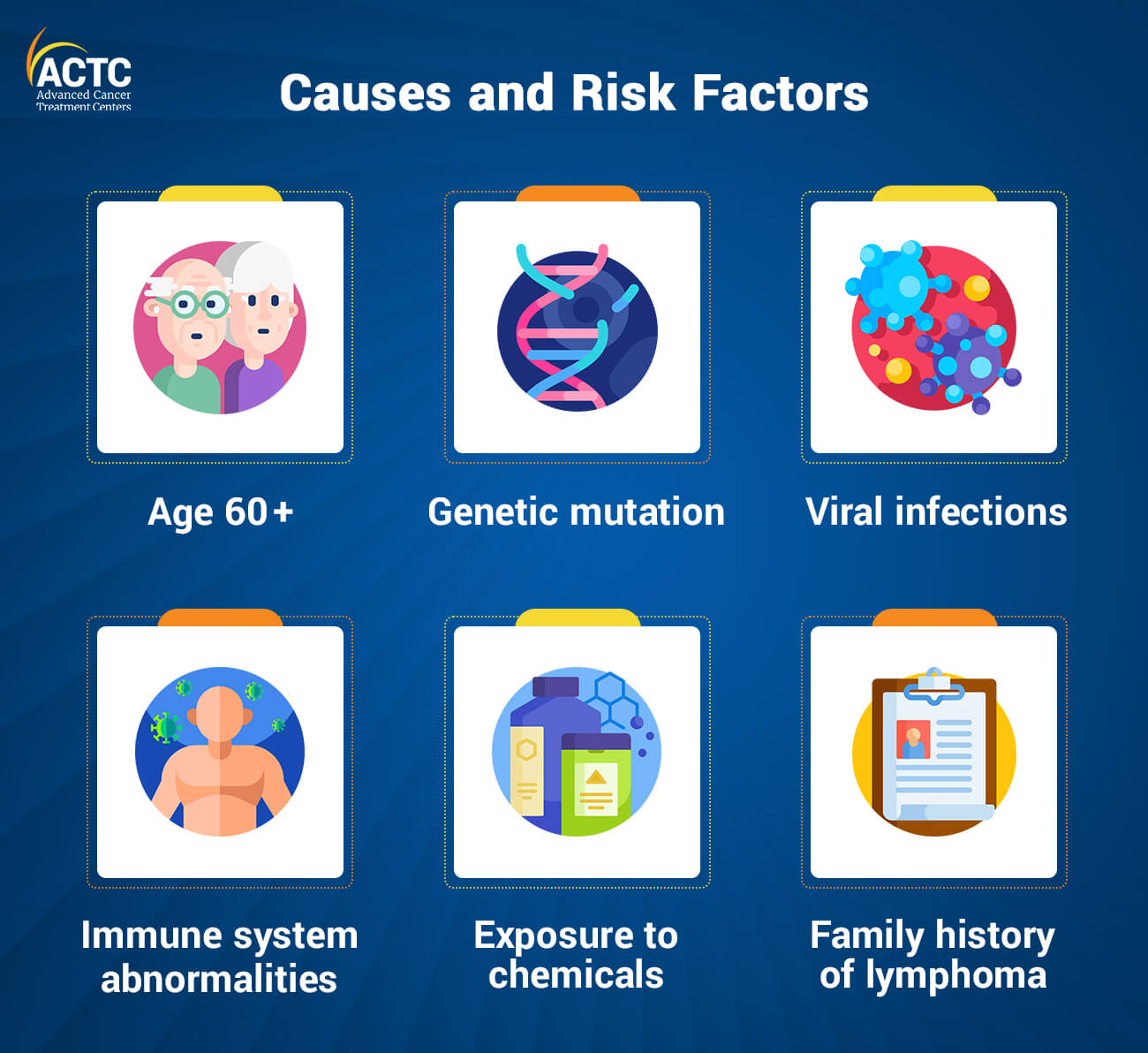
Several risk factors are associated with an increased likelihood of developing lymphoma:
- Age:
- The risk of lymphoma increases with age, particularly for NHL, which is most commonly diagnosed in individuals over 60 years old.
- Gender:
- Males are generally at a higher risk of developing lymphoma than females, although the reasons for this gender disparity are not fully understood.
- Family History:
- A family history of lymphoma or other cancers can increase an individual’s risk. Genetic predispositions, such as mutations in the BRCA1 and BRCA2 genes, are also associated with a higher risk of lymphoma.
- Infections:
- Certain viral and bacterial infections are known to increase the risk of lymphoma. These include the Epstein-Barr virus (EBV), human T-cell leukemia/lymphoma virus (HTLV-1), Helicobacter pylori (associated with gastric MALT lymphoma), and hepatitis C virus (associated with certain subtypes of NHL).
- Immune System Suppression:
- Individuals with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressive medications following an organ transplant, are at a higher risk of developing lymphoma.
- Autoimmune Diseases:
- Certain autoimmune diseases, such as rheumatoid arthritis, lupus, and Sjögren’s syndrome, have been linked to an increased risk of lymphoma.
- Environmental and Occupational Exposures:
- Exposure to chemicals such as pesticides, herbicides, and industrial solvents has been linked to a higher risk of lymphoma, particularly in individuals with long-term occupational exposure.
DIAGNOSIS OF LYMPHOMA.
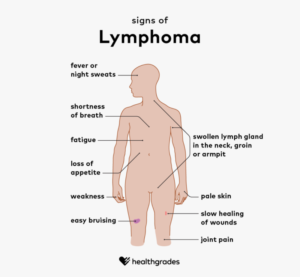
The diagnosis of lymphoma involves several steps, including a thorough medical history, physical examination, and various diagnostic tests:
- Physical Examination:
- The doctor will perform a physical examination to check for swollen lymph nodes, spleen, or liver, which are common signs of lymphoma.
- Blood Tests:
- Blood tests can help detect abnormalities in the number of blood cells, which can be a sign of lymphoma. Tests may include a complete blood count (CBC) and blood chemistry tests.
- Imaging Tests:
- Imaging tests such as X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans can help detect tumors and determine the extent of the disease.
- Lymph Node Biopsy:
- A biopsy of a swollen lymph node is the definitive test for diagnosing lymphoma. The biopsy involves removing a small sample of tissue from the lymph node, which is then examined under a microscope for the presence of cancerous cells.
- Bone Marrow Biopsy:
- In some cases, a bone marrow biopsy may be performed to determine if the lymphoma has spread to the bone marrow.
TREATMENT OPTIONS FOR LYMPHOMA
The treatment of lymphoma depends on the type, stage, and other individual factors. Treatment options may include:
- Chemotherapy:
- Chemotherapy is a common treatment for lymphoma and involves the use of drugs to kill cancer cells. It is often used in combination with other treatments, such as radiation therapy.
- Radiation Therapy:
- Radiation therapy uses high-energy beams, such as X-rays, to target and kill cancer cells. It is often used in the early stages of lymphoma or in combination with chemotherapy.
- Targeted Therapy:
- Targeted therapy involves the use of drugs that specifically target cancer cells without affecting healthy cells. For example, rituximab is a monoclonal antibody used to treat B-cell lymphomas by targeting the CD20 protein on the surface of B-cells.
- Immunotherapy:
- Immunotherapy involves the use of drugs that help the immune system recognize and destroy cancer cells. This treatment is increasingly being used for certain types of lymphoma, particularly NHL.
- Stem Cell Transplant:
- In some cases, a stem cell transplant may be used to treat lymphoma. This involves replacing the patient’s damaged bone marrow with healthy stem cells, which can be obtained from the patient (autologous transplant) or a donor (allogeneic transplant).
- CAR T-Cell Therapy:
- Chimeric antigen receptor (CAR) T-cell therapy is an advanced form of immunotherapy that involves genetically modifying a patient’s T-cells to target and kill lymphoma cells. This therapy has shown promising results in the treatment of certain types of NHL.
CURRENT RESEARCH AND FUTURE DIRECTIONS.
Research into lymphoma is ongoing, with a focus on developing new treatments and improving outcomes for patients. Some areas of current research include:
- Genetic and Molecular Profiling:
- Advances in genetic and molecular profiling are helping researchers better understand the underlying causes of lymphoma. This knowledge is leading to the development of more targeted and personalized treatments.
- Novel Therapies:
- Researchers are exploring new therapies for lymphoma, including new targeted therapies, immunotherapies, and combination treatments. These therapies aim to improve survival rates and reduce side effects.
- Clinical Trials:
- Clinical trials are essential for testing new treatments and determining their safety and effectiveness. Participation in clinical trials offers patients access to cutting-edge treatments and contributes to the advancement of lymphoma care.
CONCLUSION.
In conclusion, Lymphoma is a common and increasingly prevalent cancer that affects the lymphatic system. While the disease can be challenging to diagnose and treat, advancements in research and treatment options offer hope for patients. With continued efforts in understanding the disease and developing new therapies, the outlook for lymphoma patients is improving. Increased awareness of the commonality of lymphoma is crucial for early detection and intervention, ultimately leading to better outcomes for those affected by this disease.
RFERENCES.
- American Cancer Society. (2021). What Is Non-Hodgkin Lymphoma? Retrieved from https://www.cancer.org/cancer/non-hodgkin-lymphoma/about/what-is-non-hodgkin-lymphoma.html
- Swerdlow, S. H., Campo, E., Harris, N. L., Jaffe, E. S., Pileri, S. A., Stein, H., … & Vardiman, J. W. (2016). The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood, 127(20), 2375-2390.
- National Cancer Institute. (2020). Adult Non-Hodgkin Lymphoma Treatment (PDQ®)–Health Professional Version. Retrieved from https://www.cancer.gov/types/lymphoma/hp/adult-nhl-treatment-pdq
- Lymphoma Research Foundation. (2021). Understanding Lymphoma. Retrieved from https://lymphoma.org/aboutlymphoma/lymphoma/
- Armitage, J. O., & Gascoyne, R. D. (2018). Lymphoma—Diagnosis and Treatment. Mayo Clinic Proceedings, 93(11), 1624-1632.
- Carbone, A., Gloghini, A., & Serraino, D. (2014). Epstein-Barr virus-associated lymphomas in people with HIV. Current Opinion in HIV and AIDS, 9(5), 439-444.
Written by Fawzi Rufai, Medically Reviewed by Sesan Kareem