MPOX: ALL YOU NEED TO KNOW ABOUT

Mpox, formerly known as monkeypox, has garnered significant attention due to recent outbreaks and its potential as an emerging global health concern. This comprehensive guide aims to provide all you need to know about mpox, including its symptoms, transmission, treatment options, and preventive measures. By understanding these aspects, you can better grasp the implications of this disease and the steps necessary to mitigate its impact.
What is Mpox?
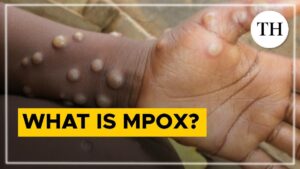
Mpox is a viral zoonotic disease caused by the mpox virus, a member of the Orthopoxvirus genus, which also includes the variola virus (which causes smallpox) and the vaccinia virus (used in the smallpox vaccine). The term “monkeypox” was derived from the virus’s initial discovery in laboratory monkeys in 1958. However, the virus can infect a variety of animals, and humans are not its primary host.
HISTORICAL BACKGROUND.
Mpox was first identified in humans in 1970 in the Democratic Republic of the Congo. Since then, cases have been reported primarily in central and western Africa. Historically, mpox has been a relatively rare disease, confined largely to rural areas of Africa where the virus is endemic. However, the landscape of mpox is changing, with recent outbreaks raising global concern.
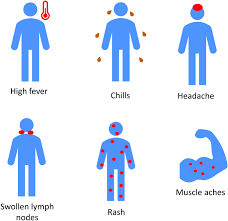
Symptoms of Mpox

Mpox presents with a range of symptoms that are somewhat similar to those of smallpox, though generally milder. The disease typically progresses through several stages, starting with flu-like symptoms and followed by a characteristic rash.
Initial Symptoms
The onset of mpox is usually marked by:
- Fever: Often one of the first symptoms, fever may be accompanied by chills and sweating.
- Headache: Persistent headaches can occur, often alongside general malaise.
- Muscle Aches: Muscular pain and fatigue are common.
- Lymphadenopathy: Swollen lymph nodes can be a distinguishing feature, as they are not commonly seen in other pox-like diseases.
Rash Development
Approximately one to three days after the onset of fever, a rash develops, typically starting on the face and then spreading to other parts of the body, including:
- Pustules: The rash progresses through macules, papules, vesicles, and pustules before forming scabs. The pustules are filled with fluid and may become crusty over time.
- Location: The rash often starts on the face and can spread to the arms, legs, palms, and soles.
The rash can be itchy and painful, and in severe cases, it may lead to complications such as secondary bacterial infections.
TRANSMISSION AND RISK FACTORS
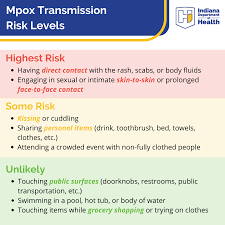
Mpox is primarily a zoonotic disease, meaning it is transmitted from animals to humans. However, human-to-human transmission is also possible. Understanding how the virus spreads can help in preventing infection.
Zoonotic Transmission
- Animal Contact: Mpox can be transmitted to humans through direct contact with the blood, bodily fluids, or lesions of infected animals. Rodents, such as squirrels and rats, are considered primary reservoirs of the virus.
- Handling Infected Animals: Individuals who hunt or handle animals in areas where mpox is endemic are at higher risk.
Human-to-Human Transmission
- Respiratory Droplets: Although less common, mpox can spread through respiratory droplets from an infected person, especially if they have a cough or are in close contact.
- Direct Contact: Contact with the rash, bodily fluids, or contaminated surfaces (such as bedding or clothing) can also facilitate transmission.
- Sexual Contact: There is evidence to suggest that mpox can be transmitted through sexual contact, particularly when lesions are present.
DIAGNOSIS OF MPOX
Diagnosing mpox involves a combination of clinical evaluation and laboratory testing. Accurate diagnosis is crucial for appropriate treatment and control measures.
Clinical Diagnosis
- Medical History: A detailed medical history, including recent travel to endemic areas and potential exposure to infected animals, is essential.
- Physical Examination: Examination of symptoms, particularly the rash and swollen lymph nodes, helps in distinguishing mpox from other similar diseases.
Laboratory Tests
- Polymerase Chain Reaction (PCR): PCR tests detect viral DNA and are the most reliable method for diagnosing mpox.
- Serology: Blood tests can identify antibodies against the mpox virus, though they are less commonly used.
TREATMENT AND MANAGEMENT.
Currently, there is no specific antiviral treatment for mpox. Management focuses on relieving symptoms and preventing complications.
Supportive Care
- Symptom Relief: Pain and fever can be managed with over-the-counter medications such as acetaminophen or ibuprofen.
- Hydration: Maintaining adequate hydration is essential, especially if fever and sweating are severe.
- Skin Care: To prevent secondary infections, it is crucial to keep the rash clean and dry.
Antiviral Medications
- Tecovirimat: This antiviral drug, originally developed for smallpox, has shown promise in treating mpox. It can help reduce the severity of symptoms and speed up recovery.
- Cidofovir and Vaccinia Immune Globulin: These treatments may be used in severe cases, though they are not universally available.
PREVENTION AND CONTROL.
Preventing mpox involves a combination of personal protective measures and public health strategies. Effective prevention is key to reducing the spread of the virus.
Personal Protection
- Avoiding Contact: Avoid contact with animals that could be infected, especially in areas where mpox is known to occur.
- Personal Hygiene: Practice good hand hygiene, including regular hand washing with soap and water or using hand sanitizer.
- Protective Clothing: Wear appropriate protective clothing when handling animals or animal products in endemic areas.
Public Health Measures
- Vaccination: The smallpox vaccine offers some protection against mpox, though its use has been limited since smallpox was eradicated. In the case of an outbreak, targeted vaccination campaigns may be implemented.
- Quarantine and Isolation: Infected individuals should be isolated to prevent further spread, and contact tracing should be conducted to identify and manage exposed individuals.
- Education and Awareness: Public health campaigns can increase awareness about mpox symptoms, transmission, and prevention measures.
GLOBAL RESPONSE AND RESEARCH

Given the recent increase in mpox cases outside traditional endemic regions, a coordinated global response is essential. International cooperation, research, and preparedness efforts play a crucial role in addressing the potential threat of mpox.
INTERNATIONAL COLLABORATION
- Data Sharing: Countries must share data on cases and outbreaks to facilitate a coordinated response and enhance global surveillance.
- Research Initiatives: Collaborative research efforts aim to develop new vaccines, treatments, and diagnostic tools for mpox. Funding and support for research are vital for advancing our understanding of the virus and improving control measures.
Preparedness Planning
- Emergency Response Plans: Developing and implementing emergency response plans ensures that countries are prepared to handle outbreaks effectively.
- Strengthening Health Systems: Investment in healthcare infrastructure, particularly in endemic regions, improves the capacity to detect, manage, and control mpox cases.
CONCLUSION.
Mpox, though historically a relatively rare disease, has the potential to impact global health significantly. With recent outbreaks and the potential for further spread, understanding mpox—its symptoms, transmission, treatment, and prevention—is crucial for managing and mitigating its effects.
By staying informed and adopting preventive measures, individuals and communities can contribute to controlling the spread of mpox. Moreover, continued research, international cooperation, and robust public health responses will be essential in addressing the challenges posed by this emerging infectious disease.
REFERENCES:
- World Health Organization (WHO). (2023). “Mpox (Monkeypox) Overview.” Link
- Centers for Disease Control and Prevention (CDC). (2023). “Monkeypox.” Link
- National Institutes of Health (NIH). (2023). “Mpox Symptoms and Diagnosis.” Link
- Mayo Clinic. (2023). “Mpox: Symptoms and Causes.” Link
- World Health Organization (WHO). (2023). “Mpox Transmission.” Link
- Centers for Disease Control and Prevention (CDC). (2023). “How Mpox Spreads.” Link
- National Center for Biotechnology Information (NCBI). (2023). “Diagnostic Testing for Mpox.” Link
- American Society for Microbiology (ASM). (2023). “Mpox Laboratory Diagnosis.” Link
- World Health Organization (WHO). (2023). “Mpox Treatment and Care.” Link
- Centers for Disease Control and Prevention (CDC). (2023). “Treatment for Mpox.” Link
- World Health Organization (WHO). (2023). “Mpox Prevention.” Link
- Centers for Disease Control and Prevention (CDC). (2023). “Preventing Mpox.” Link
- International Health Regulations (IHR). (2023). “Global Health Security and Mpox.” Link
- Global Health Security Agenda (GHSA). (2023). “Enhancing Global Health Security.” Link
- World Health Organization (WHO). (2023). “Mpox (Monkeypox) Fact Sheet.” Link
- Centers for Disease Control and Prevention (CDC). (2023). “Monkeypox Information.” Link
Written by Fawzi Rufai, Medically Reviewed by Sesan Kareem