UNDERSTANDING FEMALE INFERTILITY

Female infertility is a significant concern affecting many women globally, impacting their ability to conceive and carry a pregnancy to term. This condition can stem from various underlying causes, each of which requires a thorough diagnostic process to identify and address effectively. In this comprehensive guide, we will explore the concept of female infertility, delve into common causes, and describe the diagnostic process to shed light on this complex issue.
CONCEPT OF FEMALE INFERTILITY

Female infertility is defined as the inability of a woman to conceive after one year of regular, unprotected sexual intercourse. For women over the age of 35, the timeframe is often reduced to six months due to the natural decline in fertility with age. Infertility affects roughly one in eight couples, making it a prevalent issue in reproductive health.
Infertility in women can result from a wide range of factors, including hormonal imbalances, structural abnormalities, and lifestyle influences. Understanding these factors is crucial for diagnosing and treating infertility effectively.
COMMON CAUSES OF FEMALE INFERTILITY

Several conditions and issues can contribute to female infertility. Below, we discuss some of the most common causes, including ovulation disorders, fallopian tube problems, and uterine abnormalities.
Ovulation Disorders
Ovulation disorders are one of the leading causes of female infertility. These disorders prevent the ovaries from releasing eggs regularly, which is essential for conception. The most common ovulation disorders include:
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that affects approximately 5-10% of women of reproductive age. It is characterized by irregular or absent menstrual cycles, elevated levels of male hormones (androgens), and the presence of multiple small cysts on the ovaries. Women with PCOS often experience difficulty ovulating, which can hinder their ability to conceive.
- Hypothalamic Dysfunction: The hypothalamus, a region of the brain, plays a crucial role in regulating the menstrual cycle by producing hormones that stimulate the ovaries. Conditions such as excessive stress, significant weight loss, or excessive exercise can disrupt the hypothalamic function, leading to irregular or absent ovulation.
- Premature Ovarian Insufficiency (POI): POI, also known as premature menopause, occurs when the ovaries stop functioning normally before the age of 40. Women with POI may experience symptoms similar to menopause, including irregular periods and reduced ovarian reserve.
Fallopian Tube Problems
Fallopian tube problems can obstruct the pathway through which the egg and sperm meet, leading to infertility. Common issues include:
- Blocked Fallopian Tubes: Blocked or damaged fallopian tubes can prevent the egg from traveling from the ovary to the uterus. Causes of tubal blockage include pelvic inflammatory disease (PID), endometriosis, and previous abdominal surgeries. PID, often caused by sexually transmitted infections, can lead to scarring and blockages in the reproductive tract.
- Hydrosalpinx: Hydrosalpinx is a condition where fluid accumulates in the fallopian tubes, leading to their dilation. This fluid buildup can result from infections or previous surgeries and can impair the tubes’ ability to facilitate egg and sperm movement.
Uterine Problems
Uterine problems can also contribute to female infertility by affecting the implantation and development of a fertilized egg. Key uterine issues include:
- Uterine Fibroids: Fibroids are benign tumors that grow in the uterus and can cause a range of symptoms, including heavy menstrual bleeding and pelvic pain. Depending on their size and location, fibroids can distort the uterine cavity and interfere with implantation.
- Endometrial Polyps: Endometrial polyps are growths on the lining of the uterus (endometrium). While they are typically benign, they can affect implantation and lead to difficulties with conception.
- Congenital Abnormalities: Some women may be born with structural abnormalities of the uterus, such as a septate uterus or a unicornuate uterus. These conditions can impact the ability of the uterus to support a pregnancy.
Additional Factors affecting female infertility
Age: This is another crucial factor affecting female fertility. As women age, their ovarian reserve decreases, and the quality of their eggs declines. This natural decline in fertility accelerates after the age of 35, making conception more challenging. Additionally, women over 40 may face an increased risk of miscarriage and chromosomal abnormalities.
Lifestyle factors: such as smoking, excessive alcohol consumption, and poor diet can also impact fertility. Smoking, for instance, can affect egg quality and reduce the chances of conception. A balanced diet and healthy lifestyle choices are essential for maintaining reproductive health.
DIAGNOSTIC PROCESS FOR FEMALE INFERTILITY

The diagnostic process for female infertility involves a series of tests and evaluations to identify the underlying causes. This process typically includes the following steps:
Initial Evaluation:
The initial evaluation usually starts with a comprehensive medical history and physical examination. The healthcare provider will ask about menstrual cycles, sexual history, previous pregnancies, and any underlying health conditions. This assessment helps identify potential factors contributing to infertility.
DIAGNOSTIC TESTS
1. Hormone Testing:

Hormone testing is a fundamental part of the diagnostic process. Blood tests can measure levels of various hormones, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol, and progesterone. These tests help assess ovarian function, determine if ovulation is occurring, and identify hormonal imbalances.
2. Ultrasound Imaging:

Ultrasound imaging is used to visualize the reproductive organs, including the ovaries and uterus. A transvaginal ultrasound provides a closer view and is particularly useful for detecting conditions such as ovarian cysts, fibroids, and structural abnormalities of the uterus.
3. Hysterosalpingography (HSG):
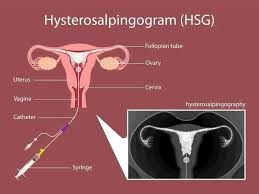
HSG is a radiologic procedure where a contrast dye is injected into the uterine cavity and fallopian tubes. This test helps assess the patency (openness) of the fallopian tubes and can identify blockages or abnormalities in the uterine cavity. HSG is often used to evaluate tubal factors contributing to infertility.
4. Laparoscopy:

Laparoscopy is a minimally invasive surgical procedure used to directly visualize the pelvic organs. During laparoscopy, a thin, lighted tube (laparoscope) is inserted through a small incision in the abdomen. This procedure allows for the examination of the ovaries, fallopian tubes, and uterus and can be used to diagnose conditions such as endometriosis or pelvic adhesions.
Additional Testing
Genetic Testing: In some cases, genetic testing may be recommended to identify chromosomal abnormalities or genetic conditions that could affect fertility. This testing is particularly useful if there is a suspicion of genetic disorders or recurrent pregnancy loss.
Endometrial Biopsy: An endometrial biopsy involves taking a small sample of the uterine lining for examination. This test helps evaluate the health of the endometrium and can identify conditions such as endometrial hyperplasia or cancer.
CONCLUSION.
Understanding female infertility involves recognizing its various causes and undergoing a comprehensive diagnostic process to identify the underlying issues. Ovulation disorders, fallopian tube problems, uterine abnormalities, and age-related factors all play significant roles in female fertility. By utilizing a range of diagnostic tests and evaluations, healthcare providers can develop effective treatment plans tailored to the specific needs of each patient.
REFERENCES:
- American Society for Reproductive Medicine (ASRM). (n.d.). Infertility and Its Causes
- Centers for Disease Control and Prevention (CDC). (2022). Reproductive Health and Infertility
- Mayo Clinic. (2023). Female Infertility: Diagnosis and Treatment
Written by Fawzi Rufai, Medically Reviewed by Sesan Kareem