Pulmonary Hypertension: A Comprehensive Overview
Pulmonary hypertension (PH) is a complex and often underrecognized condition that affects the blood vessels in the lungs, leading to increased pressure in the pulmonary arteries. This comprehensive overview will delve into the definition, causes, symptoms, diagnosis, and treatment options for pulmonary hypertension, emphasizing the importance of awareness and timely intervention.
What is Pulmonary Hypertension?
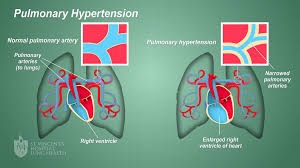
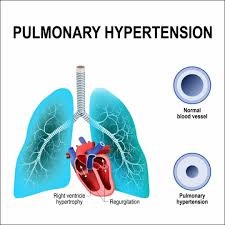
Pulmonary hypertension is characterized by elevated blood pressure in the pulmonary arteries, which transport blood from the heart to the lungs. Normal pulmonary artery pressure ranges from 8 to 20 mmHg during rest. In individuals with pulmonary hypertension, this pressure exceeds 25 mmHg at rest, or 30 mmHg during exercise, which can lead to significant health complications.
Classification of Pulmonary Hypertension
Pulmonary hypertension is classified into five groups based on the underlying cause:
- Group 1: Pulmonary Arterial Hypertension (PAH)
This includes idiopathic PAH and heritable forms, as well as PAH caused by certain drugs or toxins. - Group 2: Pulmonary Hypertension due to Left Heart Disease
This is the most common cause of pulmonary hypertension and is related to left heart failure or mitral valve disease. - Group 3: Pulmonary Hypertension due to Lung Disease and/or Hypoxia
Conditions such as chronic obstructive pulmonary disease (COPD), interstitial lung disease, and sleep apnea fall under this category. - Group 4: Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
This results from chronic blood clots in the pulmonary arteries. - Group 5: Pulmonary Hypertension with Unclear Multifactorial Mechanisms
This includes a variety of conditions that do not fit neatly into the other groups, such as sarcoidosis and certain blood disorders.
Causes of Pulmonary Hypertension

Understanding the underlying causes of pulmonary hypertension is crucial for effective diagnosis and management. Here are some common causes grouped by their classification:
1. Pulmonary Arterial Hypertension (Group 1)
- Idiopathic PAH: The exact cause is unknown, but it may involve genetic factors or abnormal blood vessel responses.
- Heritable PAH: Genetic mutations, particularly in the BMPR2 gene, can increase susceptibility.
- Drug and Toxin-Induced: Certain medications, including appetite suppressants and some chemotherapy drugs, can lead to PAH.
2. Left Heart Disease (Group 2)
- Heart Failure: Both systolic and diastolic heart failure can lead to increased pressure in the pulmonary circulation.
- Mitral Valve Disorders: Conditions like mitral stenosis can obstruct blood flow, increasing pulmonary pressure.
3. Lung Disease and Hypoxia (Group 3)
- Chronic Obstructive Pulmonary Disease (COPD): This common lung disease can lead to hypoxia and subsequent pulmonary hypertension.
- Interstitial Lung Disease: Conditions like pulmonary fibrosis can cause scarring and inflammation in the lungs, elevating pulmonary artery pressure.
- Sleep Apnea: Obstructive sleep apnea can lead to intermittent hypoxia, contributing to pulmonary hypertension.
4. Chronic Thromboembolic Pulmonary Hypertension (Group 4)
- Pulmonary Embolism: Chronic obstruction from unresolved blood clots can lead to pulmonary hypertension.
5. Multifactorial Causes (Group 5)
- Sarcoidosis: This inflammatory disease can affect the lungs and cause pulmonary hypertension.
- Blood Disorders: Conditions like sickle cell disease or thrombocythemia can contribute to elevated pulmonary pressures.
Symptoms of Pulmonary Hypertension
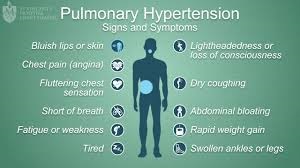
The symptoms of pulmonary hypertension can be subtle and often develop gradually, leading to delayed diagnosis. Common symptoms include:
1. Shortness of Breath
One of the hallmark symptoms of pulmonary hypertension is dyspnea, or shortness of breath, particularly during physical activity. As the condition progresses, individuals may experience shortness of breath even at rest.
2. Fatigue
Chronic fatigue is another prevalent symptom. The increased workload on the heart and reduced oxygen delivery can lead to persistent tiredness.
3. Chest Pain
Some individuals may experience chest discomfort or pain, which can be mistaken for other conditions, such as angina.
4. Dizziness or Fainting
Due to reduced blood flow to the brain, patients may experience episodes of dizziness or syncope (fainting), especially during exertion.
5. Swelling
Swelling in the ankles, legs, and abdomen can occur due to fluid retention, a consequence of right heart failure that may develop as pulmonary hypertension progresses.
6. Bluish Skin
Cyanosis, or a bluish tint to the lips and skin, may occur due to low oxygen levels in the blood.
7. Heart Palpitations
Some patients may experience irregular heartbeats or palpitations as the heart works harder to pump blood through the narrowed pulmonary arteries.
Diagnosis of Pulmonary Hypertension
Diagnosing pulmonary hypertension can be challenging due to its nonspecific symptoms. A thorough evaluation often includes:
1. Medical History and Physical Examination
A healthcare provider will take a detailed medical history and perform a physical exam, paying close attention to signs of heart failure, lung disease, and other related conditions.
2. Blood Tests
Blood tests may be performed to check for underlying conditions, such as liver or kidney function and blood oxygen levels.
3. Imaging Studies
- Chest X-ray: Can reveal enlarged pulmonary arteries or signs of heart failure.
- Echocardiogram: This ultrasound test is crucial for estimating pulmonary artery pressure and assessing heart function.
4. Right Heart Catheterization
This is the gold standard for diagnosing pulmonary hypertension. A catheter is inserted into the heart’s right side to measure pressures in the pulmonary arteries directly.
5. Pulmonary Function Tests
These tests evaluate lung function and help identify underlying lung diseases that may contribute to pulmonary hypertension.
6. Additional Tests
Depending on the suspected cause, further tests such as a CT scan of the chest, ventilation-perfusion scan, or sleep studies may be performed.
Treatment and Management of Pulmonary Hypertension

Managing pulmonary hypertension typically involves a multidisciplinary approach. Treatment goals focus on improving symptoms, enhancing quality of life, and slowing disease progression. The management strategies may include:
1. Medications
Several classes of medications are used to treat pulmonary hypertension:
- Endothelin Receptor Antagonists (ERAs): These help relax blood vessels and lower blood pressure in the lungs (e.g., bosentan, ambrisentan).
- Phosphodiesterase-5 Inhibitors: These medications improve blood flow by relaxing blood vessels (e.g., sildenafil, tadalafil).
- Prostacyclin Analogues: These are potent vasodilators that can be administered via intravenous infusion or inhalation (e.g., epoprostenol, treprostinil).
- Soluble Guanylate Cyclase Stimulators: These improve the response of blood vessels to nitric oxide (e.g., riociguat).
2. Oxygen Therapy
For patients with low oxygen levels, supplemental oxygen can help relieve symptoms and improve exercise tolerance.
3. Lifestyle Changes
Making lifestyle modifications can significantly impact disease management, including:
- Exercise: Engaging in a supervised exercise program can improve physical function and quality of life.
- Diet: A heart-healthy diet low in salt and saturated fats can help manage symptoms.
- Weight Management: Maintaining a healthy weight reduces the workload on the heart.
4. Surgical Options
In severe cases of pulmonary hypertension, surgical options may be considered:
- Atrial Septostomy: This procedure creates a small hole between the heart’s upper chambers to relieve pressure on the right side of the heart.
- Lung Transplantation: For patients with advanced pulmonary hypertension not responsive to other treatments, lung transplantation may be the only option.
5. Regular Monitoring
Patients with pulmonary hypertension require ongoing follow-up with healthcare providers to monitor disease progression and adjust treatment as needed.
Conclusion.
This is a serious condition that requires early recognition and intervention to improve outcomes. Understanding its definition, causes, and symptoms is essential for timely diagnosis and effective management. With advances in treatment options, individuals living with pulmonary hypertension can lead fulfilling lives with proper care and support.
Raising awareness of this is crucial for improving the lives of those affected and ensuring timely intervention. Regular check-ups, education, and advocacy can contribute to better outcomes and enhanced quality of life for individuals with this complex condition.
References:
- American Heart Association. (2023). “What Is Pulmonary Hypertension?” Retrieved from heart.org
- Pulmonary Hypertension Association. (2023). “Understanding Pulmonary Hypertension.” Retrieved from phassociation.org
- National Heart, Lung, and Blood Institute. (2022). “Pulmonary Hypertension.” Retrieved from nhlbi.nih.gov
- McLaughlin, V. V., et al. (2015). “Pulmonary Hypertension: A New Era.” Circulation Research, 116(5), 1-3.
- Simonneau, G., et al. (2019). “Haemodynamic Definitions and Updated Clinical Classification of Pulmonary Hypertension.” European Respiratory Journal, 53(1), 1802067.
Written by Fawzi Rufai, Medically Reviewed by Sesan Kareem